MediTelecare™ Outcomes and Research
MediTelecare™ Yields Positive Outcomes
for Skilled Nursing Facilities Through Telehealth
September 2020
By: Dr. Jessica Badichek, PharmD, BCGP
Chief Informatics & Compliance Officer
MediTelecare™ Clinical Outcomes
MediTelecare™ , the nation’s largest provider of telehealth-behavioral care to the long-term care market including skilled and assisted living centers, announced significant positive results in treating behavioral health conditions via telehealth.
From a population of over 4,500 skilled nursing facility resident-patients in over 50 facilities, facility staff referred approximately 1,350 residents to MediTelecare™ for behavioral telehealth services, (the MediTelecare™ Cohort). By treating resident-patients in this cohort, MediTelecare™ significantly reduced overall rates of inappropriate and unnecessary psychotropic medication use. Resident-patients were treated regularly on at least a 90 to 180-day protocol of telehealth sessions with an interdisciplinary team of psychologists and medical providers such as psychiatrists and nurse practitioners.
MediTelecare’s™ interdisciplinary team was often able to discontinue high-risk medications such as antipsychotics and hypnotics, successfully transitioning to either less dangerous medications or to non-pharmacologic options such as “talk therapy” to safely and effectively manage behavioral health conditions. Reducing the use of high-risk medications such as antipsychotics in turn reduces negative health outcomes such as falls with injury or other serious adverse drug events (“ADEs”), thereby reducing unnecessary healthcare costs and improving quality of care for the elderly population.
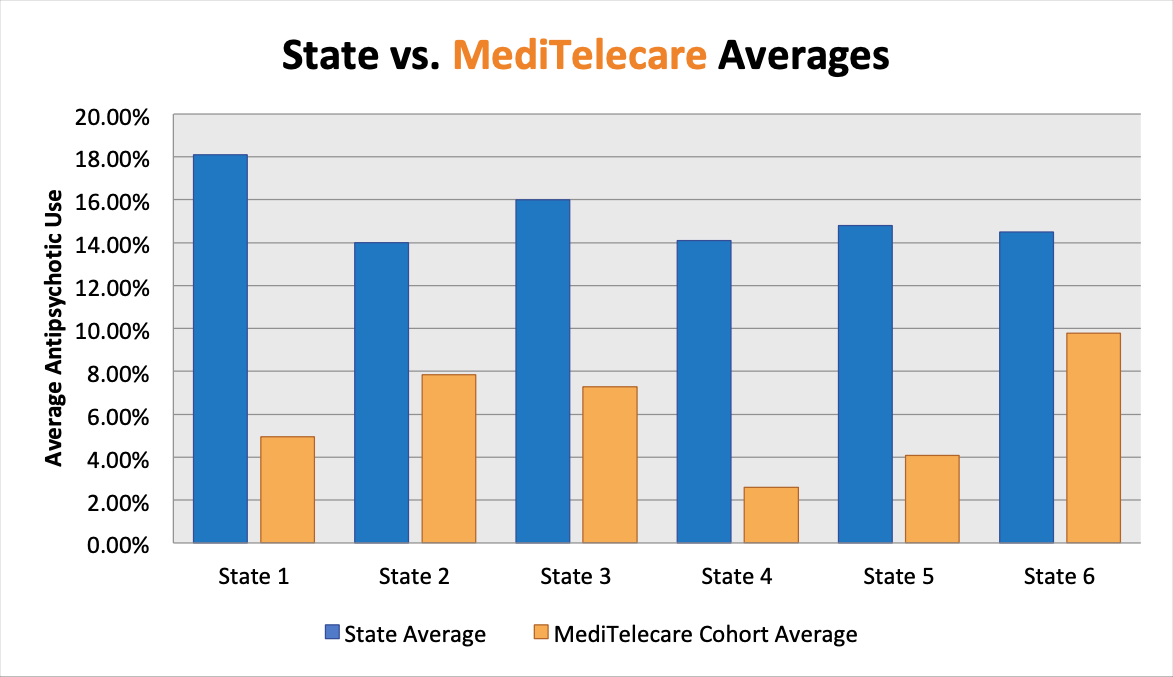
Antipsychotic Medication Use
Facilities in the MediTelecare™ Cohort averaged 7.21% antipsychotic use, just half of the 2019 National Average1 of 14.3%, by using MediTelecare™ telehealth services. In two states, cohort facilities’ rates dropped more than 70% below state averages. In every one of the cohort group of facilities, MediTelecare™ clinicians were able to achieve and maintain results significantly better than the state average. In a subgroup of over 300 resident-patients within the overall MediTelecare™ Cohort, antipsychotic use among long-stay resident-patients was even more pronounced, ranging from 32% to 64% reductions.
The overuse of antipsychotic medications in skilled nursing facilities is associated with greater medical risks for elderly resident-patients including increased mortality and serious cerebrovascular events. According to the American Psychiatric Association Practice Guideline on the Use of Antipsychotics to Treat Agitation or Psychosis in Patients with Dementia, antipsychotics should only be utilized in resident-patients with symptoms that are severe, dangerous, and/or cause significant distress to the resident-patient and when all other non-pharmacologic options have been exhausted.2 By using the MediTelecare™ standard operating protocols and a proprietary drug formulary overseen by a clinical pharmacist, MediTelecare™ clinicians can reduce inappropriate antipsychotic use that is commonly found at partnering facilities prior to commencing MediTelecare™ telehealth services. MediTelecare™ standard operating clinical protocols include replacing high-risk antipsychotics with safer alternatives such as “talk therapy” and, when applicable, more appropriate medications such as antidepressants.
Antipsychotic use is a key measurement in the Centers for Medicare and Medicaid Services (CMS) quality measures that determine a skilled nursing facility’s overall star rating signifying overall quality of resident-patient care.3
Anti-Anxiety and Hypnotic Medication Use
In addition, MediTelecare™ clinicians reduced the overall use of anti-anxiety and hypnotic medications by approximately 15% in the MediTelecare™ Cohort. Within a sub-group of over 500 resident-patients, reductions ranged from 35% to 65%.
Anti-anxiety medications such as benzodiazepines (i.e. Lorazepam, Alprazolam and Clonazepam) and hypnotic medications (“sleeping pills”) such as Zolpidem can increase the risk for falls with injury, cognitive impairment, delirium and drug dependence in elderly resident-patients. Additionally, these medications can interact with other medications such as pain medications, putting resident-patients at increased risk for serious ADE’s such as respiratory depression, coma, and even death. MediTelecare’s™ approach to resident-patients is to carefully discontinue these medications and to transition to safer, more appropriate treatments.
Anti-anxiety and hypnotic use is a key measurement in the Centers for Medicare and Medicaid Services (CMS) quality measures that determine a skilled nursing facility’s overall star rating signifying overall quality of resident-patient care.3
Overall Psychotropic Medication Use
Across the entire MediTelecare™ Cohort, telehealth clinicians were able to reduce overall psychotropic medication use in those resident-patients receiving 3 or more psychotropic drugs by approximately 17%. Psychotropic medications are psychoactive drugs affecting the mind, emotions, and behavior. MediTelecare™ clinicians using telehealth technology and standards of care can develop non-pharmacologic treatment regimens that allow resident-patients to discontinue unnecessary medications and reduce psychiatric polypharmacy.
The American Geriatrics Society's BEER'S Criteria for Potentially Inappropriate Medication Use in Older Adults recommends avoidance of 3 or more CNS (Central Nervous System) active drugs such as psychotropic medications. Such drugs can potentially increase the risk for falls, ADE’s and lead to other negative outcomes in elderly resident-patients such as increased hospitalizations.4
A study published by the American Geriatrics Society determined that falls by older adults cost the US healthcare system approximately $50 billion annually.5 The average cost of a single hospitalization for fall-related injuries is reported at approximately $30,000.6 Reducing psychotropic medications that heighten fall risk, such as antipsychotics and benzodiazepines, can help reduce these costs significantly.
Behavioral Telehealth and COVID-19
In 2020, the Coronavirus Pandemic presented many additional hurdles to effective mental health treatment in skilled nursing facilities. Resident-patients suffered increased illness and death, isolation from family and social interactions, anxiety, and depression – increasing needs for treatment. Facilities restricted visitors, and even clinicians – making it harder to provide traditional in-person treatment. These factors created the perfect environment for telehealth behavioral care to shine, providing high quality service in a highly accessible manner in the MediTelecare™ Cohort, even during the crucial first six months of 2020. By delegating behavioral health diagnosis and treatment to a successful telehealth partner, facilities could then fully focus on the coronavirus outbreak.
MediTelecare™ leadership believes these results have been achieved through a complex but reliable combination of greater access via telehealth to behavioral health specialists, who use evidence-based treatment protocols and a proprietary drug formulary. These results prove that a collaborative interdisciplinary team-based protocol using telehealth exclusively can achieve positive outcomes among a complex vulnerable resident-patient population residing in skilled centers.
- The Centers for Medicare & Medicaid Services (CMS). National Partnership to Improve Dementia Care in Nursing Homes: Antipsychotic Medication Use Data Report (October 2019). Oct. 2019, www.cms.gov/files/document/antipsychotic-medication-use-data-report-updated-01242020.pdf.
- Verduin, Marcia L. “The American Psychiatric Association Practice Guideline on the Use of Antipsychotics to Treat Agitation or Psychosis in Patients With Dementia.” Journal of Psychiatric Practice, vol. 23, no. 2, 2017, pp. 160–161., doi:10.1097/pra.0000000000000212.
- The Centers for Medicare & Medicaid Services (CMS). “About Nursing Home Compare Data.” Medicare.gov - the Official U.S. Government Site for Medicare, www.medicare.gov/NursingHomeCompare/Data/About.html.
- “American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults.” Journal of the American Geriatrics Society, vol. 67, no. 4, 2019, pp. 674–694., doi:10.1111/jgs.15767.
- Florence, Curtis S., et al. “Medical Costs of Fatal and Nonfatal Falls in Older Adults.” Journal of the American Geriatrics Society, vol. 66, no. 4, 2018, pp. 693–698., doi:10.1111/jgs.15304.
- Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. J Safety Res. 2016;58:99–103.